Fibroids are the most common growths in the uterus. Their growth is stimulated by oestrogen and progesterone, causing uterine collagen to cross-link and harden, creating a stiff mass of collagen fibres. Fibroids tend to develop in early perimenopause, when oestrogen levels increase and regress in menopause as oestrogen declines. Fibroids tend to have more oestrogen receptors, so this may be one reason oestrogen disproportionately affects the growth of these solid tumours. More than 80% of Black women and nearly 70% of white women have fibroids by age 50. Sometimes these growths are harmless and can even go undetected, but in many cases they cause symptoms ranging from pain and bleeding to infertility.
Early warning signs
The symptoms of fibroids are relatively common and can be associated with other factors or diseases, such as ovulatory dysfunction, endometriosis or endometrial polyps. Many women do not connect their symptoms to fibroids, so can go undiagnosed for some time, and some fibroids can be asymptomatic, thereby avoiding detection. Many women have uterine fibroids and don’t even know it. Small fibroids don’t often cause symptoms and don’t regularly affect your life. However, larger fibroids may lead to several warning signs, including:
- Heavy bleeding: you can experience heavy menstrual bleeding, large clots, and bleeding between cycles when you have one or more uterine fibroids. This is the most common symptom. Excessive bleeding can lead to the development of anaemia (low red blood cells) causing ongoing tiredness and weakness.
- Pelvic pressure or pain, lower back pain: pelvic pain and low back pain are common early symptoms of uterine fibroids. The pain may be sharp or feel similar to your menstrual cramps but worse.
- Full feeling in the abdomen: as uterine fibroids grow, they occupy more space in your uterus and pelvic area. You may feel like your belly is full, as if you’ve eaten a large meal.
- Increased urination: you might feel like you have to urinate more often when you have uterine fibroids. This happens when the fibroid is big enough to put pressure on your bladder. Although rare, fibroids can also cause obstruction of the ureter, which might require treatment if this progresses to severe hydronephrosis.
- Pain during sex: the fullness in your abdomen that fibroids cause can also lead to discomfort during sex. Not everyone feels this, but if you have pain with intercourse, getting evaluated for uterine fibroids is a good idea.
- Gastrointestinal symptoms: constipation or the recurrent need to void bowels can also be caused by fibroids.
- Rarely, a fibroid can cause sudden, serious pain when it outgrows its blood supply and starts to die. Get medical care right away if you have severe bleeding from the vagina or sharp pelvic pain that comes on fast.
There are long-term complications that can affect the integrity of the endometrium, the uterine lining. This means it can be difficult getting pregnant. During pregnancy, women with fibroids have an increased risk of complications compared with women without fibroids, including
- preterm delivery (16.7% versus 6.3%) and
- premature rupture of membranes (14.3% versus 2.1%)
- risk of placental abruption (7.5% versus 0.9%)
- fetal malformation (6.2% versus 3.3%)
- caesarean section (70–76% versus 32.8%)
- postpartum haemorrhage (33% versus 6%) and
- foetal malpresentation (19% versus 4.4%) are increased in women with fibroids
Fibroids can also be associated with miscarriage.
The symptoms of fibroids are relatively common and can be associated with other factors or diseases, such as ovulatory dysfunction, endometriosis or endometrial polyps. Many women do not connect their symptoms to fibroids, so can go undiagnosed for some time, and some fibroids can be asymptomatic. Lack of symptoms does not necessarily mean lack of inflammation, so women experiencing infertility should be evaluated to the presence of fibroids.
Presentation and Diagnosis
Diagnosing fibroids is usually done by transvaginal ultrasound, although this is limiting if the uterus extends beyond the pelvis, a common problem with this disease. Abdominal ultra-sonography might be required to diagnose fibroids that extend beyond the effective range of the trans-vaginal probe, but then MRI is generally preferred.
Women often have more than one fibroid. They can be different in size and in their location. The location of fibroids directly affects the symptoms they induce, as well as the time to the manifestation of such symptoms. For example, submucosal fibroids that bulge into the uterine cavity seem to have more of an effect on abnormal menstrual bleeding and pregnancy problems. This is independent of fibroid size as small fibroids that protrude into the uterine cavity can also induce menstrual irregularities. Conversely, subserosal fibroids that form on the outside of the uterus are slow growing and considerable time is needed before they are of a sufficient bulk to cause symptoms, such as back, leg or pelvic pressure and abdominal and pelvic pain.
The International Federation of Gynecology and Obstetrics (FIGO) has established a classification system which uses an 8-point numerical system to describe the location of fibroids relative to the endometrium (submucosal surface) and the serosal surface, with low numbers indicating a central location.
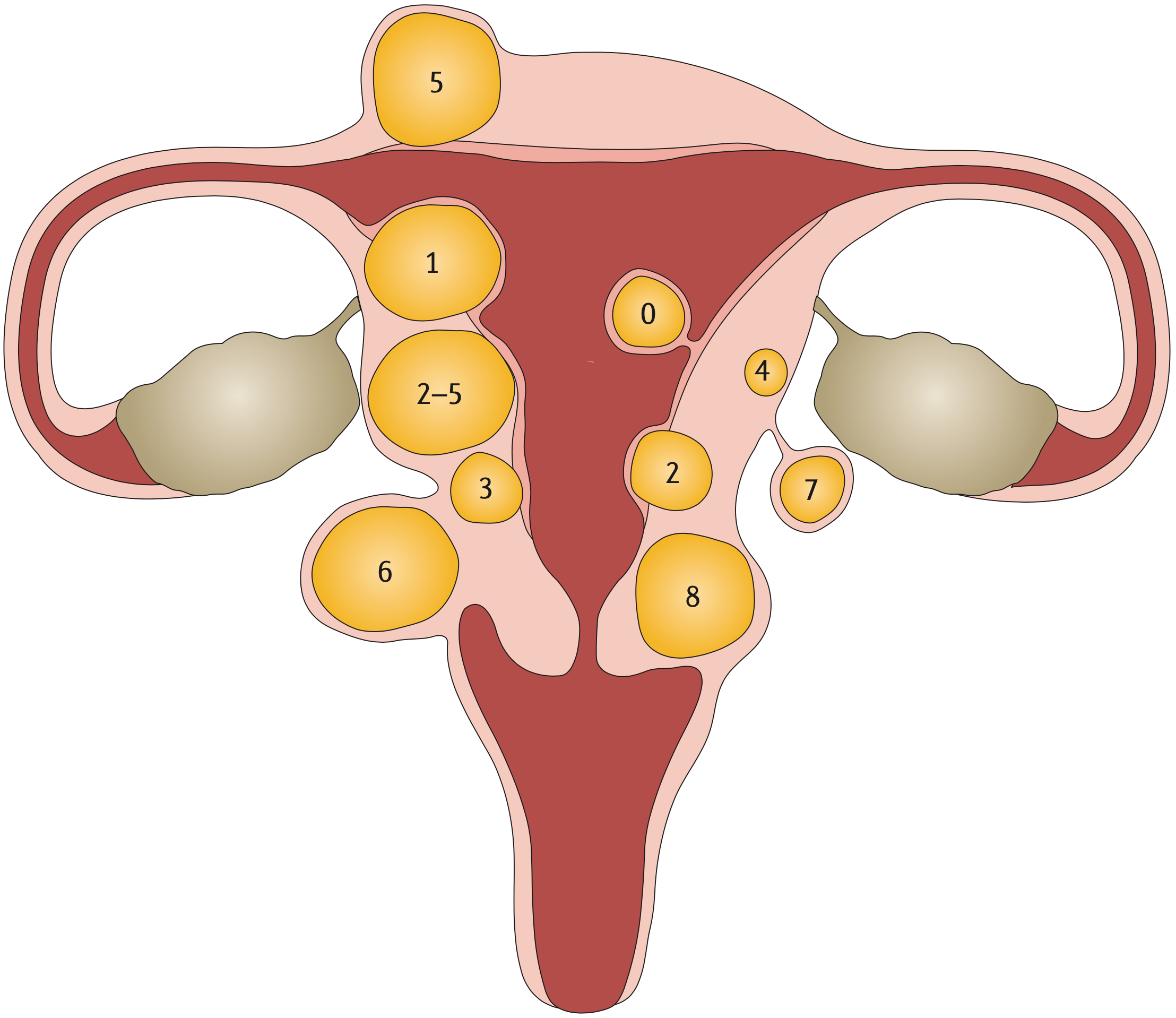
- Type 0: pedunculated fibroid, which is localized in the submucosa and extends inside the uterine cavity
- Type 1: submucosal fibroid, with <50% in an intramural location
- Type 2: submucosal fibroid, with ≥50% in an intramural location
- Type 3: contacts the endometrium, with 100% in an intramural location
- Type 4: intramural fibroid
- Type 5: subserosal fibroid, with ≥50% in an intramural location •
- Type 6: subserosal fibroid, with <50% in an intramural location •
- Type 7: subserosal pedunculated fibroid
- Type 8: other (for example, cervical or parasitic)
Recently, shear wave elastography (SWE) has been developed as a potential screening tool for the early identification of women at risk for developing fibroids. This provides the option of preventative treatment to delay or even arrest or reverse fibroid progression.
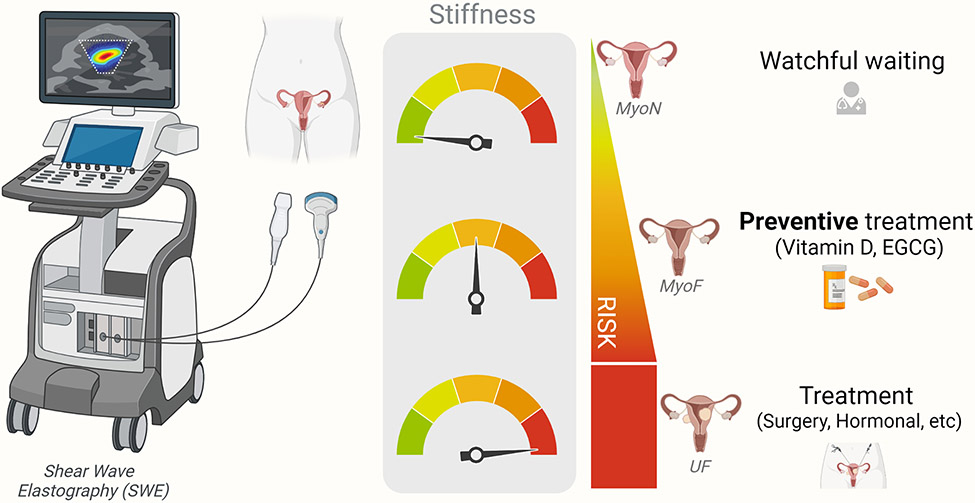
Proposed application of SWE as a screening tool for identification of women at risk of fibroid development and corresponding preventive measures to be taken. MyoN: normal non-fibroid myometrium; MyoF: at risk-myometrium, EGCG: Epigallocatechin Gallate.
The principle of SWE is to use sound waves to produce images. The sound waves can give an indication of how stiff the uterine tissue is: soft, firm, solid or hard. The stiffness indicates the progression of fibroid growth, as well as the use of appropriate therapies.
Biomarkers
In urine
As oestrogen can fuel the growth of fibroids, it can be helpful to identify whether oestrogen is elevated, and how it’s metabolised. DUTCH urine testing is unique because it helps identify symptoms of hormonal imbalances by providing a complete picture of hormone levels which cannot be seen in testing serum (blood) alone. The DUTCH test can measure the levels of the 3 types of oestrogen, oestrone (E1), oestradiol (E2) and oestriol (E3) and how they are metabolised.

Estradiol (E2) is the most biologically active estrogen in the body. However, estrone (E1) and the phase 1 estrogen metabolites (2-OH, 4-OH, 16-OH) can also bind to estrogen receptors. Thus, it is possible that elevations in any of these markers may contribute to fibroid growth.
The phase 1 metabolite, 16-OHE1, tends to bind more tightly to oestrogen receptors than the 2-OH and 4-OH metabolites (but not nearly as tightly as E2), and is known to cause tissue groeth. If too much oestrogen is metabolised into the 16-OHE1 form, it may contribute to increased fibroid growth.
Having this information is extremely valuable, because it means that as a practitioner I can first reduce the amount of oestrogen and alter the metabolism of oestrogen in a more favourable way.
In blood
The CA-125 blood test measures the amount of CA125 protein that both women and men have in their blood. CA-125 is elevated in cases of fibroids, endometriosis and adenomyosis, as well as ovarian cancer. This means that it can’t be used to identify any one of these conditions, but it can be used to monitor progression.
Development and Progression of Fibroids
Fibroids are associated with high oestrogen levels, or oestrogen dominance. Obesity and the perimenopausal state are often associated with higher oestrogen levels. Studies have shown that oestrogen levels are actually higher in perimenopausal women, and fat is hormonal organ capable of producing oestrone, a strong oestrogen. The inflammatory mediators interleukin-2 (IL-2), IL-6, tumor necrosis factor-alpha (TNF-alpha), and leuko- triene B4 (LTB4) are also produced in the adipocyte and contribute to fibroid formation.
MED12 gene mutations created by high oxidative stress in the uterus drive fibroid formation
Nearly 70 percent of uterine fibroids are linked to a mutation in the MED12 gene but recreating this problem in the lab has proven to be difficult because when cultured, the mutant cells in the fibroids do not survive. This year scientists used CRISPR-based genome editing technology (for which 2 women scientists won a Nobel prize in 2020) to precisely engineer cells that have the same mutation in the MED12 gene. After successfully culturing the mutated fibroid cells in 3D spheres, it was found that the cells produced heightened levels of collagen, a key feature of uterine fibroids, as well as other chromosomal abnormalities commonly seen in uterine fibroids.
A clear connection has been made between MED12 mutations and high levels of oxidative stress in the uterus. The direct connection between oxidative stress and MED12 is not yet clear however almost all the risk factors below can drive oxidative stress.
Risk Factors
Anything that increases oestrogen:
- Age
Increasing age is a significant risk factor for uterine fibroids, especially among women at the premenopausal stage and those ≥ 40 years of age. For instance, 60% of African American women aged 35-49 years reported uterine fibroids, whereas 80% of those aged ≥ 50 have uterine fibroids. Among White women, 40% of those aged ≤ 35 years and 70% aged ≥ 50 years developed uterine fibroids. Rapid growth of fibroids after the age of 30, especially in perimenoause, is consistent with age-related changes in oestrogen and progesterone. Fibroids have not been detected in prepubertal girls, and only sporadic cases have been reported in adolescents. However, the factor(s) involved in their development at such an early age is unknown. Due to the slight difference in biochemical pathways, uterine fibroids in young women do not exhibit typical uterine fibroid biology. In several cases, adolescent patients had a translocation between chromosomes 12 and 14, which is a confirmed risk factor for uterine fibroids. Women at the menopausal stage have shrunk uterine fibroid lesions and decreased sex hormones. - Early first period
Women with an earlier age at menarche had higher levels of estradiol and estrone and lower levels of sex hormone-binding globulin than women with a later age at menarche. - Early use of oral contraceptives
Use of oral contraceptive for the first time between 13 to 16 years of age increases the risk of fibroids - Excessive sugar
Elevated 2-hour glucose post-challenge, an indicator of diabetes, is found to be associated with an increased risk of fibroids. Sugar boosts oestrogen levels and is strongly associated with a higher risk of breast cancer.
Sugar boosts insulin which can increase the conversion of testosterone to oestrogen via the enzyme aromatase. Fibroids express three times higher aromatase levels than surrounding tissues, increasing active estradiol promoting growth of fibroids. - Soy
Babies fed soy formula within 2 months of birth and for more than 6 months had an elevated risk of fibroids incidence in comparison with those never fed soy formula. Additionally soya is associated with an increased risk of uterine fibroids in premenopausal women. - Red meat?
A diet higher in protein is protective however there has been a question mark around the risk of red meat increasing oestrogen. A study measuring the concentrations of oestrogen in American and Japanese beef found that the median concentrations of E2 and E1 in USA beef fat were 140 times and 11 times, respectively, higher than those in Japanese beef fat. In red meat, E2 and E1 levels of USA beef were ∼600 times and 10 times, respectively, higher than those of Japanese beef. It’s likely that the very high levels of E2 and E1 in American beef derive from the steroids given to the cattle. On the other hand, nearly zero level of E2 seen in Japanese beef was considered to be the natural endogenous status in beef without steroids. The go on to say “Accordingly, it is our intuitive feeling that the increasing consumption of oestrogen-rich beef following steroid implantation might facilitate oestrogen accumulation in the human body and could be related to the incidence of hormone-dependent cancers”, and very likely fibroids. - HRT
A state-of-the-art literature review found that some combinations of oestrogen and progestin have exhibited a significant influence on fibroids enlargement, as well as in frequency of newly detected fibroids in menopause. By contrast, several studies failed to demonstrate a significant increase in fibroids size, although a trend towards enlargement was noted. Women should have regular thorough follow-up, including trans-vaginal ultrasound for the monitoring of fibroid size, and HRT should be discontinued if an increase in size of uterine fibroids is documented. - Obesity
Fat tissue, has been proven to play hormonal, metabolic, and immune regulatory roles in the body. Fat cells make leptin, a hormone which in excess can promote inflammation driving fibroid growth. Additionally fat cells create a fibroid-friendly micro-environment that can induce fibrosis and fuel fibroid growth by increasing blood supply to it. Each kilogram of excessive body weight is correlated with an increased risk of uterine fibroids development. A study conducted in the United States found that women diagnosed with uterine fibroids are heavier than those without uterine fibroids. Moreover, an increase in the body mass index (BMI) by one unit, higher waist-to-hip ratios, and body fat percentage exceeding 30% increase the risk for uterine fibroids. Abdominal visceral fat also enhances this risk. Obesity and particularly excess visceral fat may be complemented with the reduced production of the sex hormone-binding globulin (SHBG), which binds circulating hormones, disrupting the hormonal activity toward sensitive tissues, and thereby influencing the delicate hormonal balance in the body. - Alcohol
Alcohol and especially beer are known to increase oestrogen. A recent Korean study assessed alcohol consumption and the risk of new-onset fibroids in 2.5 million Korean women aged 20 to 39 years concluded:- Mild-to-Moderate Drinkers vs. Heavy Drinkers: Women who consumed alcohol had a higher chance of developing uterine leiomyomas. The increase in risk was between 12% and 16%. Specifically, women who drank alcohol mildly to moderately had about a 12% higher risk, while heavy drinkers had about a 16% higher risk.
- Frequency of Drinking: The risk of developing these tumors increased with the frequency of alcohol consumption. Women who drank once a week had an 11% increased risk, while those who drank three or more times a week had a 15% increased risk.
- Amount of Alcohol per Session: The risk also increased with the amount of alcohol consumed per session. Drinking seven or more glasses of alcohol in one session was associated with a 17% increased risk.
- Sustained Drinkers vs. Sustained Non-Drinkers: Women who consistently consumed alcohol over a period of time (referred to as “sustained drinkers”) had a 20% increased risk of developing these tumors compared to women who consistently did not drink alcohol (referred to as “sustained nondrinkers”).
- Change in Drinking Habits: Women who stopped drinking alcohol showed a small increase in risk (3%), whereas women who started drinking who previously did not have a 14% increased risk.
In summary, the study found that drinking alcohol is associated with a higher risk of developing uterine leiomyomas, and this risk increases with the amount and frequency of alcohol consumption. Women who consistently drink have a notably higher risk compared to those who don’t drink or those who stopped drinking.
- An imbalanced gut microbiome
The estrobolome is a collection of bacteria in the gut which is capable of metabolising and modulating the body’s circulating oestrogen. The gut bacteria regulate oestrogens through secretion of β-glucuronidase, an enzyme that splits detoxified oestrogen, releasing free oestrogens that are then reabsorbed into the bloodstream and repeatedly circulated through the body, increasing oestrogen levels. The genes for β-glucuronidase are widely found in Firmicutes (which are increased in the vaginal microbiome in women with fibroids, see below).

Possible mechanisms that could link gut dysbiosis and the development of uterine fibroids.
A dysbiotic gut results in an altered microbiome which triggers the following pathways
- interferes with the estrobolome functioning and results in hyperestrogenic state leading to uterine fibroids
- altered levels of gut metabolites such as short chain fatty acids (SCFA) which triggers immune dysregulation and induce inflammation and also leads to hyperestrogenic state
- interferes the gut permeability leading to a leaky gut and toxicity which could dysregulate the immune function.
- COMT
Catechol-O-methyltransferase (COMT) is an enzyme that triggers enhanced transformation of 2-hydroxyestradiol (anti-estrogen) into 2-methoxyestradiol (pro-estrogen) with resultant hyperestrogenic environment that may contribute to cell proliferation and increase in fibroid development. High COMT activity has been found in fibroids. Women with the high-activity COMT Val/Val genotype are 2.5 times more likely to develop fibroids than women with other genotypes. The prevalence of this genotype was significantly higher in African American women (47%) compared with white (19%) or Hispanic (30%) women. - MTFHR
Methylenetetrahydrofolate reductase (MTHFR) plays a key role in the enzymatic process in the folate metabolism pathway, which converts folic acid (obtained from food and/or supplements) into methyl-folate (the form of folate used by your body), and then participates in DNA synthesis, modification and methylation. The mutation of the MTHFR C677T gene leads to the disorder of folate metabolism, the decrease of antioxidant capacity, the increase of uterine related oxidative stress, and the proliferation of uterine smooth muscle cells, thus leading to the formation of fibroids. Additionally MTHFR mutations can cause high blood pressure via increased homocysteine. Vitamin B2 (riboflavin) is a required cofactor for MTFHR and higher vitamin B2 levels are associated with increased MTHFR enzyme activity, lower homocysteine and improved blood pressure.
Genetic testing has identified:- The wildtype (non-variant) MTHFR 677 shown as “CC”. This is associated with 100% enzyme activity and does not increase risk for higher homocysteine or high blood pressure.
- A single MTHFR 677 variation shown as “CT”. This results in 30-35% reduction in enzyme activity and can slightly increase risk for higher homocysteine levels and blood pressure.
- A double MTHFR 677 variation shown as “TT”. This results in 60-70% reduction in enzyme activity and increases the risk for higher homocysteine and high blood pressure.
Prolactin
Fibroids are associated with high prolactin levels, originating from the fibroid itself or from the pituitary gland. High prolactin can cause infertility and fibroid progression.
Blood pressure (hypertension)
A study this year reported that women with untreated hypertension faced an 18% higher risk of developing uterine fibroids when compared to those without hypertension. Conversely, women with hypertension who were using blood pressure medications had a 37% lower risk of developing uterine fibroids, with the use of angiotensin-converting enzyme inhibitors associated with a 48% lower risk. Interestingly, women with new-onset hypertension had a 45% greater risk of uterine fibroid diagnosis, while those with pre-existing hypertension had little additional risk. The formation of fibroids is attributed to the chronic destruction of the uterine lining due to increased blood flow and inflammation.
Vitamin D deficiency
A systematic review last year concluded that 100% of all research studies identified vitamin D deficiency in women with uterine fibroids. The best estimate of the effect of hypovitaminosis D on fibroid development found that deficient vitamin D (< 20 ng/mL) increased the risk of uterine fibroids by 32%. The importance of this relationship is underscored by the prevalence of vitamin D deficiency, a condition which affects approximately 80% of Black American women, a population disproportionately affected by fibroids.
Further, a case-control study this year found that vitamin D supplementation reduces fibroid growth and development, perhaps partly because it reduces COMT activity.
Further, vitamin D recovers the damaged DNA repair system, thus inhibiting fibroid progression.
Women at risk for deficiency should be screened and those with deficiency should take supplements. The functional range for vitamin D is 125-150. I usually recommend 10,000 IU a day at deficiency below 60 and test serum levels regularly to avoid any overdose-related toxicities. Routine vitamin D supplementation for women with insufficiency may provide effective treatment and prevention of fibroids.
Imbalanced vaginal microbiome
A recent study showed that an increased level of the bacterial phyla Firmicutes was observed in both the cervical and vaginal microbiome of women with fibroids. An increased level of Firmicutes is associated with obesity. Firmicutes include Lactobacillus, Streptococcus, Clostridia, and can be reduced with high animal protein diet.
Uterine infections
Fibroids are associated with Chlamydial infection, and pelvic inflammatory disease. The risk of fibroids is increased 5x when infections are associated with the copper coil.
Copper Intrauterine Devices (IUD)
The copper coil may be a cause of uterine fibroids. Intrauterine devices can cause local irritation, pressure, inflammation, and tissue changes in the uterus. Copper IUDs in particular impact cellular mechanisms in the endometrium. There may be oedema, vascular congestion, cell death, and other cytological alterations. These effects involve inflammatory cytokines and changes in cell proliferation and activity that have been associated with fibroids: Interleukin 1 beta (IL-1β) and tumour necrosis factor-alpha (TNF-α) levels were high in the late secretory phase and IL-6 levels were high in the proliferative early secretory phase in IUD-subjected endometrial samples. The expression of IL-1, IL-6, and TNF-α was found to be associated with the pathophysiology of uterine fibroids. A study concluded that the use of copper IUDs for more than 2 consecutive years should be avoided in order to prevent oxidative damage.
Copper T380A is one of the most commonly prescribed IUDs and has been shown to significantly increase copper levels. The use of copper T-200 IUD for 12 months significantly increased copper levels and significantly decreased zinc and iron levels. It is suggested that the low zinc status was probably responsible for the heavy bleeding which was common among the study group using copper IUDs, which in turn was responsible for the anaemia seen in more than 50% of the IUD users.
The adverse effects of copper intrauterine devices (IUDs) such as abnormal bleeding, pain and cramps may be due in part to the burst release of copper ions during the first few months of usage. Copper can then continue to build up slowly in the body. Coppertoxic.com reports: “For many women, symptoms often first begin appearing 2 or 6 months after insertion. For others, the time period may be much longer, years to decades, before they notice anything, or connect the dots. Side effects of the copper IUD as copper accumulates usually begin with increasing brain fog and fatigue, often paired with a racing mind. Eventually, once the liver is overloaded, copper will then start accumulating more in the brain, and severe shifts in personality can occur as a result of increasing bio-unavailable copper and calcium and changes in neurotransmitter production. The period 2 to 5 months post-insertion is a common time for many women when metabolism begins slowing and energy, behaviour, and reactions begin changing, especially with a tendency towards increasing depression and irritability.”
Zinc was found to be decreased and copper increased in the blood serum of women with diagnosed uterine fibroids compared to the control tissues, which may be associated with PMS in the luteal phase of the menstrual cycle.
Estrogen is known to increase copper absorption vice versa. Having an excess of copper in the body has been linked to being one of the key underlying drivers of anxiety, oestrogen dominance, painful periods, heavy periods, irregular periods, mental health issues, and overall hormonal imbalances.
Toxic pollutants
Common chemicals called phthalates found in hundreds of household products have been linked to fibroids. Phthalates are present in many household items ranging from food packaging and processing equipment to shower curtains, building materials, and car interiors. Phthalates are also used as solvents in cosmetics and other personal care products and to coat or encapsulate certain pharmaceutical pills and dietary supplements. The chemicals can leach out of these products and enter food, air, and water, meaning you can swallow, inhale, or absorb these phthalate particles through direct skin contact. The body then metabolises these chemicals, yielding byproducts that several studies have detected in human urine, breastmilk, and blood.
DEHP, a phthalate that’s commonly added to plastics to make them flexible has been found to foster the survival and growth of fibroids, helping them grow to large sizes. DEHP has been found to enhance MED12, triggering fibroid formation.
Studies connect in utero exposure of those women who are going to develop uterine fibroids while the foetus is still in the uterus. When those women are exposed to endocrine-disrupting chemicals — compounds you can find in plastics, beauty products — those endocrine-disrupting chemicals can disrupt the hormonal signalling. And, later in life, the children of those women who are exposed to endocrine-disrupting chemicals have a higher chance of developing uterine fibroids.
In the meantime, in November this year L’Oreal announced that one of the recipients of its 2023 For Women in Science Fellowship program is Joscelyn Mejías, whose research in biomedical engineering at John Hopkins University focuses on studying uterine fibroids. She hopes her research will lead to new and better treatment options for targeting uterine fibroids and fibrosis. Perhaps L’Oreal should also focus on removing toxins from their products.
Racial Disparities
A systematic review and application of social, structural, and political context to racial disparities in uterine fibroids found that Black women face worse clinical and surgical outcomes than their white counterparts. The differences in gene expression in fibroids from Black and white women, as well as racial disparities in fibroid prevalence, they say, may reflect that Black individuals disproportionately experience exposures linked with increased risk for uterine fibroids.
This includes a higher risk of chronic psychological stress, adverse childhood experiences, perceived racism and environmental contaminant exposures like air pollution among Black women, which have all been associated with a higher risk for developing and experiencing severe symptoms from fibroids.
Racial disparities may also stem from other social determinants of health such as a higher fat diet, lower levels of physical activity, vitamin D deficiency, as well as individual behaviours such as use of chemical hair relaxers that contain chemicals that are associated with increased risk of uterine fibroids. Studies have also suggested racial disparities in uterine fibroids and endometriosis can be linked to a lack of adequate access to health care, authors note, including minimally invasive gynecologic surgeons, interventional radiologists, and bias and discrimination within the health care system. “Black women may be more likely to have symptoms dismissed, report negative experiences with the health care system and wait too long to see a specialist, which delays diagnosis and treatment,” the author said. “These significant differences in experiences, access and dismissal or misattribution of symptoms may lead to worse outcomes.”
While some women with fibroids don’t have symptoms, others have significant pain, anaemia, heavy menstrual bleeding, increased urinary frequency, fertility problems and pregnancy complications. Black women are diagnosed with fibroids roughly three times as frequently as white women, develop them earlier in life and tend to experience larger and more numerous fibroids that cause more severe symptoms. The author of the study said “If we are sincere about striving for health equity, then we have to look at the underpinnings of inequity in our healthcare system and in society. Solutions need to address root causes of disparities through policy, education and programs that ensure all patients receive competent care.”
Associations
Association with Breast Lumps (fibroadenoma)
The same mutated MED12 gene that is found to cause fibroids is also found in 59% of breast fibroadenomas. This indicates that benign tumours of the breast and uterus, both of which are key target tissues of oestrogen, may share a common genetic basis underpinned by highly frequent and specific MED12 mutations. Interestingly supplementing with iodine resolves breast lumps and breast pain which may indicate that iodine deficiency is also a driver for fibroid development.
Tissues that store iodine include the thyroid, breasts, ovaries, uterus and placenta. While the thyroid tends to concentrate a higher percentage of iodide (I¯), other tissues tend to utilise a greater percentage of molecular iodine (I₂), which exerts multiple and complex actions related to its role as an antioxidant, an anti-inflammatory, a pro-inflammatory, an inducer of cell death, an immune modulator, and a promotor of cell differentiation. Importantly, iodine helps to maintain the oestrogen balance in favour of estriol which has been shown to protect against oestrogenic cancers and decrease the risk of fibrocystic changes in the breasts.
High oestrogen levels can prevent the absorption of iodine, which may be an additional cause of fibroid development. Iodine deficiency has been associated with fibrocystic breast disease and, more recently, with the development of distant metastatic breast cancer in young women aged 25-39. This trend toward the development of breast cancer in younger women has been associated with the reemergence of iodine deficiency in the U.S. since the 1970s. Since iodine protects against abnormal cell development and proliferation, adequate iodine levels may prevent fibroids from occurring.
Association with Breast Cancer
Both the uterus and breasts have sex hormone dependence, and this year a study involving over 630,000 women concluded that women with fibroids have a higher risk of breast-related diseases, including cancer:
- Benign breast disease: 33.5% higher risk
- Carcinoma in situ : 79.6% higher risk
- Breast cancer: 30% higher risk
Women with fibroids should be more vigilant about breast cancer, having regular breast exams and ultrasound for early detection of breast cancer.
Advances in Surgical Treatment
Traditional surgical treatments for fibroids are:
- Removing the whole womb including the fibroids (a hysterectomy). This is an option for
women who do not want to have any (more) children. - Removing the fibroids only (called myomectomy). This type of operation is suitable for women
who want to keep their uterus – mainly to preserve the chance for future pregnancy.
More recent surgical treatments for fibroids include:
- Removing the fibroid through keyhole surgery (laparoscopic myomectomy).
- Blocking the blood vessels feeding the fibroids (uterine artery embolization) which does not
remove fibroids but can cause them to shrink and reduce heavy periods. - Some fibroids that are growing inside the the womb can be removed through a hysteroscope passed inside the womb through the cervix.
There are many factors to consider when deciding the best way of removing fibroids. These include the number of fibroids, their size and exactly where they are in the womb. There can also be other issues to consider like whether you have had any operations on the womb in the past. For example, some of the fibroids that grow inside the womb can be removed by using hysteroscope operations. The fibroids that are more embedded in the womb itself cannot be removed this way.
In the last few years some hospitals have been offering SONATA: Sonography-Guided Transcervical Fibroid Ablation. It is an incisionless, uterus-preserving, transcervical approach, with real-time visualisation using intrauterine ultrasound guidance, and combines ultrasound imaging with radiofrequency energy.
Recently scientists have been developing a new therapeutic treatment using a drug capable of breaking fibroids down inside the body. Since fibroids are collagen-based, the key ingredient in this intervention is collagenase, an enzyme that digests collagen, and it is combined with LiquoGel™, which is liquid at room temperature, and becomes a gel at body temperature. Because of that, once it gets injected into a fibroid, it becomes a gel. Over time, collagenase will degrade the fibroid and LiquoGel™ will degrade, allowing the body to get rid of it. Much work remains before the treatment can reach patients.
Tests to Consider for Evaluation Fibroids
| Transvaginal and abdominal ultrasonography | To determine the size and location of fibroids and rule out ovarian tumors |
| Progesterone/estradiol ratio (100–300:1) Luteal phase progesterone measurement | Low luteal phase progesterone level support oestrogen dominance and fibroid growth |
| Vitamin D test | Low levels increase fibroid growth by several mechanisms |
| Vitamin A test | Low levels shown to increase heavy bleeding |
| Iron or total iron-binding capacity measurement, ferritin tests | Low iron stores reduce uterine contractions and increase menstrual blood loss |
| Zinc and copper tests | An imbalanced copper:zinc ratio can lead to fibroids |
| Thyroid function testing | Hypothyroidism associated with menstrual dysfunction |
| MTFHR testing | 35% weakness in methylation, increased oestrogen dominance |
| DUTCH testing for Phase 1 and Phase 2 oestrogen detoxification evaluation | Unhealthy oestrogen metabolism contributes to oestrogen dominance |
| Comprehensive digestive stool analysis | Intestinal dysbiosis is a cause of oestrogen dominance through several mechanisms |
| Vaginal microbiome testing | An unbalanced vaginal microbiome has been associated with fibroids |
| Testing for celiac disease (antigliadin antibodies) | Gluten grain sensitivity common in fibroid sufferers and can lead to further oestrogen dominance |
My approach to treating fibroids
My personal experience with fibroids, and supporting women with fibroids, clearly shows that nutrition, supplements and lifestyle changes can make a significant impact on fibroid size, heavy bleeding and pain to the point of not creating any symptoms. I initially ask clients to commit to a 3-month trial period, during which they will do as much of their protocol as possible. At the end of these first 3 months, we assess symptoms, such as heavy bleeding and pain, and any growth or shrinkage of the fibroids. The protocol is considered successful if the client perceives a reduction in symptoms and no further fibroid growth has occurred. We then continue the program for 3-month periods while continuing to monitor symptoms and uterine size. If at any time symptoms recur or worsen or the fibroids begin to grow, other more aggressive measures must be considered.
Nutrition
Women with fibroids begin a hormone-balancing diet involving foods with low inflammation effects, low acidity, and a low glycemic load.
Reduce foods that increase oestrogen dominance:
- Foods that are acidic and inflammatory, like red meat, poultry, and dairy, contain arachidonic acid. This acid can increase inflammation and help fibroids grow. Avoiding commercial meat products also reduces exposure to added hormones. Small amounts of range-fed meats can be added back once inflammation goes down.
- Sweets and high glycemic foods can cause stress and raise insulin. This can increase oestrogen dominance and help fibroids grow. Eating breakfast with protein, fat and quality carbs prevents drops in blood sugar. This avoids spikes in cortisol and adrenaline, which break down muscle and raise insulin resistance.
- Gluten grains like wheat, rye and barley contain a strong gluten that is genetically engineered. This gluten can raise oestrogen by blocking the detoxifying cytochrome P450 3A4 enzyme system. It can also affect thyroid hormones. Anyone with high oestrogen should be tested for gluten sensitivity.
- Alcohol, dairy, coffee, artificial ingredients, colours, flavours and preservatives should be avoided. Also avoid margarines and foods with trans fats or hydrogenated oils.
Include foods that reduce oestrogen dominance:
- Cruciferous vegetables such as broccoli, Brussels sprouts, cabbage, and cauliflower support healthy oestrogen metabolism.
- 3 cups of green tea daily are helpful (to reduce COMT activity).
Gut and Vaginal Microbiome Restoration, and Detoxification
- Healing intestinal and vaginal microbiome imbalance and supporting liver detoxification restores hormone balance and remove sources of inflammation.
Supplements
These nutrients to support hormone metabolism and reduce inflammation:
- Vitamin B complex, methylated
- Vitamin D
- Vitamin A
- Indole-3-carbinol or diindolylmethane (DIM) to reduce estrogen dominance
- Aromatase inhibitors such as Myomin can reduce oestrogen dominance
- Calcium D glucarate can reduce increased recirculation of oestrogens from the gut back into the body
- Iodine
- Calcium: significant negative associations have been found between low serum calcium levels and uterine fibroids, uterine size and the number of fibroid nodules, possibly reflecting associated low vitamin D levels
- Selenium has been shown to reduce fibroid size, possibly because it is an integral part of the antioxidant enzymes glutathioneperoxidase, catalase, and superoxide dismutase (SOD) which neutralise oxidative toxic intermediates, and of which there is a deficiency in fibroids.
- Iron, copper/zinc, and manganese are also required for optimum antioxidant activity.
Lifestyle
- Support for weight loss to maintain an appropriate weight.
- Avoidance of toxic xenoestrogens (dioxins, polychlorinated biphenyls) by eating organic foods and avoiding plastics
- Having regular exercise
Takeaways
- Being over 40 with heavy periods may be a strong sign of having fibroids, and the risk is higher in Black women
- Silent fibroids may be a cause of infertility
- Oestrogen and progesterone are drivers of fibroid onset and growth
- Fibroid growth is largely mediated by high levels of oxidative stress in the uterus via the MED12 gene
- DUTCH testing can identify elevated oestrogen and unbalanced oestrogen metabolism
- Increased risk with obesity (more than 30% body fat increases risk), drinking alcohol, having high blood pressure
- Increased risk with chemicals commonly found in plastic and cosmetics.
- Increased risk with imbalanced gut and vaginal microbiomes
- Increased risk with genetic variants of COMT and MTFHR genes
- A hormone balancing diet is essential
- Multiple supplements are supportive in prevention and treatment particularly iodine and methylation support
- Routine vitamin D supplementation for those with insufficiency provides effective treatment and prevention
- Women with fibroids should be more vigilant about breast cancer, having regular breast exams, or ultrasound for early detection of breast cancer
- HRT and the copper coil may increase the risk of fibroid onset and progression